There are no proven therapies that prevent or treat Long COVID. Christmas Eve, however, brought the world a promising gift. On December 24, follow-up results from the COVID-OUT trial were released, which offer the tantalizing possibility that a well-known diabetes drug could prevent the development Long COVID.
The COVID-OUT study was a randomized placebo-controlled trial that tested whether existing therapies could be repurposed as an early treatment for COVID. Three drugs were tested: metformin (a diabetes drug), ivermectin (an anti-parasitic I have previously written about), and fluvoxamine (an anti-depressant). The study enrolled overweight subjects age 30-85, with a median age of 45. The primary goal of the study was to see if any of these drugs could prevent the development of severe COVID when taken early in the course of infection. Previously published results have shown that not to be the case for any of them, although metformin might have benefit in preventing the worst outcomes.
A secondary outcome of the trial was whether patients received a formal diagnosis of Long COVID. Participants were followed for up to 10 months after their infection and asked whether their doctor had given them such a diagnosis. This endpoint was added after the start of the trial but pre-specified before results were available.
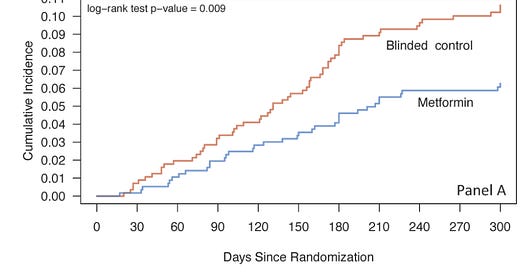
Participants who received two weeks of metformin at the start of their infection were about half as likely to later receive a diagnosis of Long COVID, compared to those who had received a placebo. The confidence interval spanned a 12% to 62% reduction in risk. Neither ivermectin nor fluvoxamine offered a benefit.
This trial has a lot going for it—mainly its gold standard design. Metformin is also a cheap, safe drug. Taking a short course of it to prevent a potentially devastating outcome seems like something many patients would be willing to do. There is reason, however, to be cautious.
Long COVID is a challenging entity to define. The disease encompasses a range of symptoms and severity. There is no diagnostic test for Long COVID, and we have only the most rudimentary understanding of its biological underpinnings. COVID-OUT mostly side-stepped these issues by going with provider diagnosis. The fact that a physician treating the patient rendered this diagnosis is meaningful, but not infallible. There will surely be over- and under-diagnosis. Furthermore, we don’t have a good sense of what Long COVID looked like in the study subjects. In the original trial results, none of the therapies reduced symptoms better than placebo during the initial infection. The best course of action is a follow-up study dedicated to this question, with careful long-term tracking of symptoms and severity.
You might have heard that the antiviral Paxlovid can prevent Long COVID. Not quite. The study that reported this finding was not a randomized trial; it was retrospective and observational. The overconfidence with which these findings were disseminated was embarrassing. This is simply not how we practice medicine. Paxlovid is authorized for the prevention of severe disease among high-risk individuals who are early in the course of their infection. This is its only RCT-proven benefit, and there are open questions about how well it will work in the setting of widespread immunity. I have written about this issue for The Atlantic.
Congratulations to the COVID-OUT study authors on a major development in the fight against Long COVID, and a note of gratitude to the participants who volunteered for the trial.
Thanks for subscribing,
Ben




Great article, thank you! I’m excited to find another trustworthy and well informed medical voice here on Substack... for a while it seemed like the antivax, ivermectin crowd had a stranglehold. I think they are still more profitable...
I’m guessing the benefit of metformin won’t hold up as well in non-obese patients. What is your guess?
I also don’t discount the potential benefit of paxlovid as much purely based on the less ideal study design. Unless you’re over 65, the main concern with Covid illness should be long haul symptoms (disabling for some) and the consequent rise in cardiovascular events for at least a year after diagnosis. That’s what I’m seeing in my practice, a rise in cognitive problems, heart attacks, pulmonary emboli... anecdotally I know, but still... the endothelial damage of covid makes it a systemic nightmare.
I’ve been a hopeful early adopter of paxlovid treatment ever since a 90% reduction in viral load was announced in the initial trial. That has to be good, right? And the 26% reduction in long covid seen in the VA study was in older individuals mostly >60, a population less likely to develop PASC than the middle aged crowd.
Enjoyed your article in The Atlantic (I subscribe), and will follow your writing from here on out. Thanks for a great post!
Thanks for this article! I was wondering if you could speculate on the mechanism by which metformin would affect Covid disease processes.